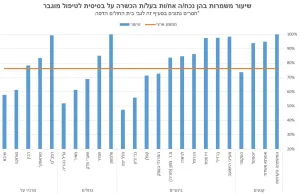
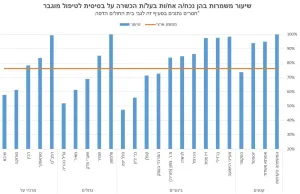
Public Notice From Niach Nature Y.S. Ltd. Regarding the Product: “Faran – Organic Day Moisturizing Cream
Faran Organic Day Moisturizing Cream label omits mandatory Limonene allergen warning. Consumers with fragrance sensitivity are advised to avoid use.